Story by Lisa Rowell
March is National Sleep Awareness Month, reminding us of the importance of getting a good night’s sleep, and the potential risks of sleep disorders. This month’s Clean Living series focuses on sleep hygiene and practices for improving sleep quality. You don’t need to lay awake all night wishing you could sleep like a baby when there’s help for disordered sleeping.
The Sleep Foundation (sleepfoundation.org) estimates that 42.1 percent of Kentucky adults get less than seven hours of sleep each night. This is the third highest sleep deprived state, with Hawaii taking the top spot and West Virginia in close second.
The site indicates that nearly half of those with below-average sleep quality rated their mental health as poor or very poor.
The Sleep Foundation offers some tips on their website to try to get a better night’s sleep. These include techniques such as slow, deep breathing; meditation practices; progressive muscle relaxation; imagery; the military sleep method which was designed to help service members fall asleep in tense situations; and other methods worth taking a look at if you’re barely getting in 40 winks on a regular basis.
Sleep hygiene
While our younger selves may have been able to party into the wee hours on a Saturday night, or burn the midnight oil on a project, and be ready for work or school Monday morning, it seems the older we get, the harder it is to bounce back from a lack of sleep.
The experts at the Sleep Foundation tell us that practicing good sleep habits to support healthy sleep can make a huge difference. These can include:
- Getting at least 30 minutes of natural light early in the day.
- Maintaining a consistent sleep schedule.
- Optimizing your bedroom environment for sleep.
- Avoiding caffeine at least eight hours before bed.
- Avoiding alcohol at least four hours before bed.
- Limiting screen time before bed.
Chronic sleepless nights could be an indicator of an underlying medical condition and you should consult your primary care practitioner to rule out medical issues or to see if a sleep study is right for you.
Sleep studies

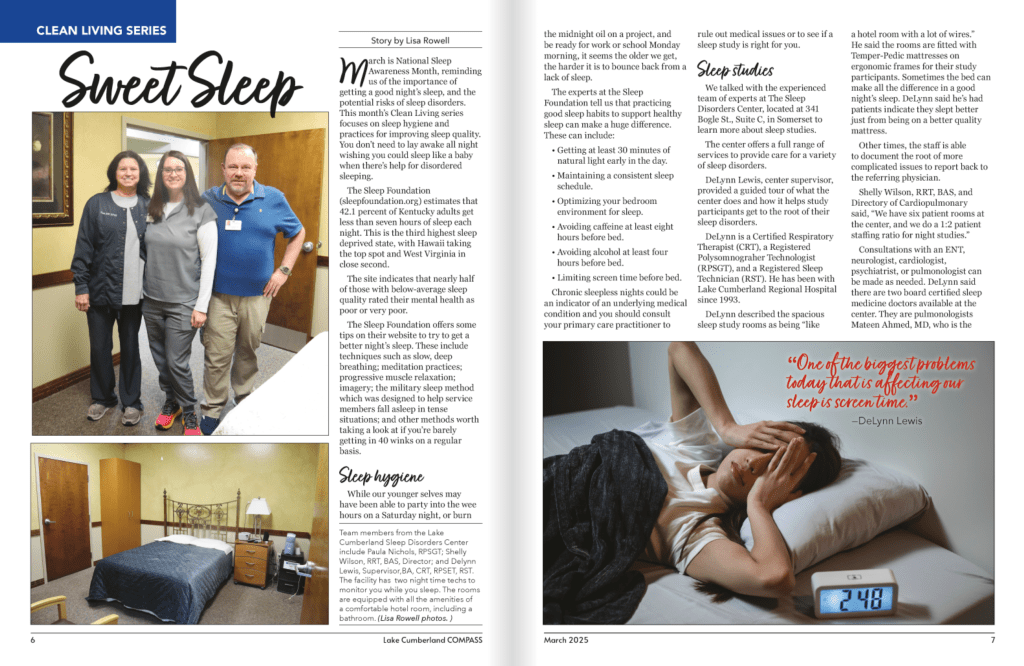
Team members from the Lake Cumberland Sleep Disorders Center include Paula Nichols, RPSGT; Shelly Wilson, RRT, BAS, Director; and Delynn Lewis, Supervisor,BA, CRT, RPSET, RST. The facility has two night time techs to monitor you while you sleep. (Lisa Rowell photo)
We talked with the experienced team of experts at The Sleep Disorders Center, located at 341 Bogle St., Suite C, in Somerset to learn more about sleep studies.
The center offers a full range of services to provide care for a variety of sleep disorders.
DeLynn Lewis, center supervisor, provided a guided tour of what the center does and how it helps study participants get to the root of their sleep disorders.
DeLynn is a Certified Respiratory Therapist (CRT), a Registered Polysomnograher Technologist (RPSGT), and a Registered Sleep Technician (RST). He has been with Lake Cumberland Regional Hospital since 1993.
DeLynn described the spacious sleep study rooms as being “like a hotel room with a lot of wires.” He said the rooms are fitted with Temper-Pedic mattresses on ergonomic frames for their study participants. Sometimes the bed can make all the difference in a good night’s sleep. DeLynn said he’s had patients indicate they slept better just from being on a better quality mattress.
Other times, the staff is able to document the root of more complicated issues to report back to the referring physician.
Shelly Wilson, RRT, BAS, and Directory of Cardiopulmonary said, “We have six patient rooms at the center, and we do a 1:2 patient staffing ratio for night studies.”
Consultations with an ENT, neurologist, cardiologist, psychiatrist, or pulmonologist can be made as needed. DeLynn said there are two board certified sleep medicine doctors available at the center. They are pulmonologists Mateen Ahmed, MD, who is the medical director of the center, and Sandy Schuldheisz, MD.
DeLynn also said not all sleep studies need to be conducted in-lab at the center. Home sleep tests can also be used to evaluate certain sleep disorders.

The study rooms at the Sleep Disorders Center are equipped with all the amenities of a comfortable hotel room, including a bathroom. (Lisa Rowell photo)
Sleep centers or laboratories in Kentucky are required to be accredited to operate. The Sleep Disorders Center is accredited by the Accreditation Commission for Health Care (ACHC).
“We’re a very busy lab,” DeLynn said of the center. “Last month we did 96 procedures which included in-home and lab studies.”
Sleep studies at the center are done by physician’s referral. DeLynn said the in-lab studies generally last one night. They accept patients as young as three years old.
He said the home studies are specific to sleep apnea and have a different set of criteria. Patients come in for an interview that lasts about 30-45 minutes and they are fitted for the equipment which they take home and bring back the following day.
Disorders
DeLynn said most people think of sleep apnea when it comes to sleep disorders, however he said there are many other disorders.
Insomnia is a symptom that may be caused by several factors from physiological to environmental. The hospital’s website indicates these can include “restless legs” syndrome, nocturnal myoclonus, sleep apnea and gastrointestinal disease. The site further outlines that anxiety and stress, either situational or chronic, are also frequently implicated in insomnia. The use of depressants, stimulants, shift work, time zone changes or general discomfort may also be causative.
In DeLynn’s multi-decade experience with sleep studies, he said he can often tell if a person is more predisposed to having sleep apnea — where a person stops breathing during sleep — by the appearance of a recessed lower jaw. Sleep apnea is a sleep disorder characterized by repeated episodes of breathing cessation or shallow breathing during sleep. It can be caused by excess weight or obesity, enlarged tonsils or adnoids, a large tongue, narrow upper airway, or neck muscles that relax too much during sleep.
DeLynn said in addition to the CPAP machines we’re familiar with, there is also the Inspire implant for treating sleep apnea. It can be implanted by an ENT as an outpatient surgical procedure. The implant monitors breathing patterns and sends mild pulses to the tongue, which move it away from the throat, in turn keeping the airway open.
Loud snoring may be a symptom of serious sleep apnea which can occur several hundred times over the course of one night. Sleep apnea may lead to high blood pressure, heart rhythm disturbances and excessive daytime sleepiness (EDS).

From drowsiness during quiet situations to drastic impairment of daytime functioning, excessive daytime sleepiness (EDS) can often lead to accidents. Reduced alertness may be temporary such as in severe respiratory allergy or prolonged when due to sleep apnea and narcolepsy. Other underlying medical conditions such as encephalitis, drug abuse or metabolic disease may be cause EDS.
Parasomnias happen in a state between sleep and wakefulness. Common in children, parasomnias can also occur in adults. They include things such as sleep walking, bed wetting, night terrors, clenching or grinding of the teeth, or head banging.
DeLynn said narcolepsy is more common than one would think.
“It’s a grossly underdiagnosed disorder,” he said.
Besides having an irresistible urge to sleep, narcoleptics often suffer from sleep paralysis, a sudden and brief episode of muscle weakness referred to as “cataplexy,” or hypnagogic hallucination.
Narcolepsy can be objectively diagnosed at the sleep center, with daytime as well as nighttime testing to document REM at sleep onset.
There are a host of other sleep disorders that may be long-term or temporary, such as jet lag or sleep deprivation. DeLynn said they’ve seen some unique disorders such as REM behavior disorder (acting out dreams during REM sleep stage). He said this could be an early indicator of other health problems.
DeLynn said the Sleep Disorders Center has also been able to help identify non-sleep related issues such as cardiac problems through their extensive and thorough monitoring.
Screen time
DeLynn agrees about the importance of good sleep hygiene with “setting regular bedtimes, setting regular wake times, and just getting on a schedule.”
“One of the biggest problems today that is affecting our sleep is social media,” he said. “We are too wired to our phones.”
Shelly added, “Even if you’re reading with a Kindle, you’re still getting that screen time.” She added that blue light blocking methods could be helpful.
Screen time, whether it’s from our phones, video games, or the television, especially when it’s close to bedtime, disrupts the body’s natural sleep-wake cycle. The blue light emitted from screens suppresses the production of melatonin, making it harder to fall asleep. DeLynn said needing to sleep with the television on is a bad habit.
“Screen time is a problem but also you need a quiet, secure place to sleep,” DeLynn said.
Other tips for better sleep
DeLynn agrees with the Sleep Foundation’s advice for better sleep hygiene and adds the following tips: “Something I’ve found that helps me — and I’m someone that has to have a quiet room — I like my white noise from my air purifier and ceiling fan,” DeLynn said, adding, “but also deep breathing.”
“I would not recommend caffeine past lunch,” DeLynn advised. This is also a protocol for sleep study participants who have a pre- and post-questionnaire associated with the study.
Kids and sleep
DeLynn was adamant about the importance of good sleep for our children. “If a child is not getting adequate good sleep, their growth development is retarded. Their ability to thrive is delayed. Their ability to comprehend is also affected.”
All of the good sleep hygiene habit adults should follow are equally as important for our kiddos. Speak with your child’s health care provider if you notice any abnormalities in his or her sleep patterns.
Sleep stages
According to the Sleep Foundation, sleep is not uniform. It’s made up of several rounds in the sleep cycle, each consisting of four stages — three non-rapid eye movement stages and one rapid eye movement stage. A person typically goes through four to six rounds of these stages in a typical night. The duration of the stages can vary.
The sleep stages allow the brain to recuperate from the day and they also support multiple functions.
The first stage of sleep is brief and lasts just a few minutes. It occurs as a person first falls asleep. Although a person can be easily awakened from this stage, if left undisturbed, he or she will quickly move into the second stage of sleep, where the body enters a more subdued state. This stage can last for 10 to 25 minutes during the first sleep cycle, with each stage becoming longer during the night. Collectively, a person typically spends about half their sleep time in the second stage of sleep.
The third stage of sleep, known as N3 or deep sleep, is harder to awaken from. As the body relaxes, the brain activity goes into a pattern known as delta waves, which experts believe is critical to restorative sleep and may also bolster the immune system and other key bodily processes. Even though brain activity is reduced, there is evidence that deep sleep contributes to insightful thinking, creativity, and memory.
The Foundation states that a person spends the most time in deep sleep during the first half of the night. During the early sleep cycles, the N3 stages can commonly last for 20 to 40 minutes. As you continue sleeping, these stages get shorter, and more time gets spent in REM sleep instead.
Not all sleep cycles are the same length, but on average they last about 90 minutes each.
During rapid eye movement (REM) sleep patterns, brain activity picks up. The body experiences “atonia,” which is a temporary paralysis of the muscles, with two exceptions: the eyes and the muscles that control breathing. REM sleep is believed to be essential to cognitive functions like memory, learning, and creativity.
Although dreams can occur during any sleep stage, our most vivid dreams occur during REM sleep.
Under normal circumstances, the sleeper enters REM stage after being asleep for about 90 minutes. As the night goes on, REM stages get longer, especially in the second half of the night. While the first REM stage may last only a few minutes, later stages can last for around an hour. In total, REM stages make up around 25 percent of sleep in adults.
Sleep stages are important because they allow the brain and body to recuperate and develop. Failure to obtain enough of both deep sleep and REM sleep may explain some of the profound consequences of insufficient sleep on thinking, emotions, and physical health. Sleepers who are frequently awoken during earlier stages, such as people with sleep apnea, may struggle to properly cycle into these deeper sleep stages. People with insomnia may not get enough total sleep to accumulate the needed time in each stage.
If you’re struggling to get a good night’s sleep on a regular basis or feel you may be suffering from a sleep disorder, talk with your primary care practitioner.
Promote healthy sleep habits, such as establishing a regular sleep schedule, creating a relaxing bedtime routine, and avoiding blue screens, caffeine and alcohol before bed. ν
For more information about the Lake Cumberland Sleep Disorders Center, visit: lakecumberlandhospital.com/sleep-disorders-center
Sources: The Sleep Foundation (SleepFoundation.org); National Library of Medicine, Biotech Information; The National Center for Biotechnology Information advances science and health by providing access to biomedical and genomic information.
